|
After listening to our last Five Minute Friday episode, ACL Tears, The Basics!, one of our patients wanted to know what to expect after a surgical ACL repair. As discussed in that episode, ACL tears are commonly repaired with graft surgery - taking the tissue of another tendon in the body and sewing it to the damaged ACL tendon. Like any other procedure, swelling is to be expected. Also, it should be no surprise that you will have difficulty with knee extension (straightening and bending your knee). Something that may come as a surprise is what's called an extensor lag - the inability to contract your quadriceps. This means you’ll have difficulty lifting your leg. But this is very common and you will regain contraction in about a week or two after surgery. This is something that will be worked on in physical therapy as well. Will you need crutches or a brace after surgery? You will use crutches for about 1 - 2 weeks after surgery as full weight bearing is increased throughout your rehab. ACL protocols vary but patients usually begin walking without crutches anywhere around day three to week two. Usually you will go from two crutches to one and eventually phasing them out completely. Whether or not you are given a brace after surgery is dependent on your surgeon. Typically, if given a brace after surgery, you will have a bigger, bulkier one - one that is locked in place and only unlocked at physical therapy. As you progress through your rehab, a smaller unlocked brace will be given to you. What are the most important aspects of rehab? Activating your quadriceps and regaining your knee extension are very important aspects of ACL rehab. This is because knee extension (bending and straightening the knee) influences your gait and ability to walk, climb stairs, etc. The number one thing that a patient needs to gain after ACL reconstruction surgery is quadriceps strength. Without it you will not be able to progress to higher levels of activity and your mobility will be limited. Knee range of motion is also very important… Full knee range of motion is also an important aspect of a successful rehab. After surgery you will have a very limited range of motion. The goal is for you to have your full range of motion back around the 6 - 8 week mark. During week 1 - 2 you and your physical therapist will work on getting you to a 90° angle. Week two - six you will progressively work on gaining a full range of motion (140°). Thanks for reading! Stay tuned for more information in the coming weeks.
0 Comments
Did you watch the super bowl? Did you hear the announcers say “ACL”? Joe Burrow, the starting quarterback for the Cincinnati Bengals tore his ACL two years ago, and during the game, former New York Giants wide receiver (currently on the LA Rams) Odell Beckham Jr. tore his! ACL stands for Anterior Cruciate Ligament. What is it? It’s one of the primary ligaments in the knee, along with the Posterior Cruciate Ligament (PCL) Medial Collateral Ligament (MCL) and Lateral Collateral Ligament (LCL) So how does an ACL tear? The majority of ACL tears come from non-contact injuries - when a person themselves places great force or movement on their knee to cause injury. They can also tear with contact injuries which is when there is a valgus force (force from the side) on the knee from the force of another person. In field sports a big culprit of non-contact ACL tears is from what we call the “turf monster”. This is when the turf catches the person’s foot while they’re running or trying to come to a stop on the field. Which is how Odell Beckham Jr. tore his ACL. There is also an increase in ACL tears among women, most likely due to the Q Angle (The angle between the hip and knee) - something that we will touch on in more depth on another Five Minute Friday episode. Rehab for an ACL tear typically involves surgery as there is poor blood supply to this ligament. Therefore, it’s unlikely to re-heal itself. ACL tears are generally replaced by a graft of another tendon, such as:
Generally a return to sports is a 9 month timeline, obviously there are always outliers (Adrian Peterson) but 9 months is a framework that most protocols revolve around. We will go more in depth of return to sport on another episode of 5 Minute Friday. Stay tuned! Thanks for reading! By: Dr. Tony Tanzi, PT, DPT, CSCS and Dr. Kyle Ioos, PT, DPT  You're fresh out of surgery and you arrive to physical therapy in your sling. You're not allowed to move your arm but your physical therapist is... This is what we call manual therapy. It's when a physical therapist is doing any skilled intervention (treatment) with their hands. There are 3 main reasons to do manual therapy: Reduce Pain Improve tissue tension Improve mobility / range of motion These are all great to do at the early stages of treatment, meaning in your first few visits due to the higher level of pain you are experiencing. As your pain decreased we will transition you off of manual therapy and onto more functional based exercises. We broke down manual therapy into six different types: 1. Passive Range of Motion: This is when a Physical Therapist is moving your limb through a motion and you are totally relaxed, letting the therapist do all the work. 2. Joint Mobilization This is when the Therapist will try to loosen a specific joint capsule, again with you the patient being totally relaxed 3. STM or MFR Soft tissue massage or Myofacial release are two types of “massages” to relieve tissue tension. 4. Transverse friction massage This is usually performed across a healed scar or over scar tissue in a “transverse” direction to aid in breaking up scar tissue. 5. Strapping A massage is done on a muscle while there is movement. 6. Effleurage Primarily used to decrease swelling of the limbs in post surgical patients. This type of manual therapy gently attempts to circulate the swelling back into the system. Manual therapy is NOT what we would call instrument assisted therapy (IASTM). This type of therapy is when a Therapist uses tools (graston tools, cupping tools etc) to assist with the manual techniques. It is important to note that manual therapy is best used at the early stages of your treatment. As you progress it is vital to transition to more functional based activities and exercises. This helps you the patient regain independence and get back to living an active lifestyle! By: Dr. Kyle Ioos, PT, DPT and Dr. Tony Tanzi, PT, DPT, CSCS “I have pain that starts in my low back and goes down my leg, what is it?
Ah, yes, good old - SCIATICA! What is sciatica you ask? Sciatica is nerve pain in your lower back that radiates down your leg and is caused by an irritation, inflammation or pinching of a nerve in the lower back. The most common cause is a herniated disc or slipped disc. Did you know? The sciatic nerve is the longest and thickest nerve in the body. What does Sciatic pain feel like? Sharp, shooting, jolt, burning, electric or even jabbing pain that travels anywhere from your buttock down to your toes. But I have pain in both legs, is that Sciatica? Although it is unlikely to be affecting both legs, it CAN happen. Does sciatica happen suddenly or slowly over time? Both - Sciatica can come on suddenly or gradually. It all depends on the cause. A disk herniation will cause sudden pain where arthritis in the spine will develop slowly. Who is at risk for sciatica? - Anyone with a previous back injury - any injury to your lower back puts you at risk. Overweight - Increased weight or load on your spine can lead to back strains and pains Lack of core muscles - the core is what protects your spine and gives you support. Manual labor or active jobs - heavy lifting / bending puts you at high risk Have osteoarthritis - any damage to your spine will compromise the nerves Inactive lifestyle - prolonged sitting or not being active can make your muscles stiff can increase your risk Pregnant women - certain hormones of pregnancy cause loosening of ligaments making the spine less stable What are the common causes of Sciatica? Herniated or slipped disc Degenerative disk disease (natural wear down of the discs between the vertebrae of the spine) Spinal stenosis (narrowing of the spinal canal) How do you diagnose Sciatica? PTs use what's called a Straight Leg Raise Test MDs can use: X-rays MRIs Nerve Conduction Velocity test How is Sciatica Treated? Various manual techniques, stretches and exercises all go into a proper sciatica plan of care. If you or someone you know are suffering from Sciatica pain or discomfort, text BACKPAIN to (845) 225-2000 and I will send you a video with 3 simple exercises to help alleviate or reduce your pain! Don’t wait, text BACKPAIN to our number (8452252000) and you can get started in reducing your discomfort! We get this all the time:
“On my script it has ultrasound checked off. I just want to know what is ultrasound and what is it used for?” There are two types of ultrasound: Diagnostic and Therapeutic. Diagnostic: Sound waves are used to create a real time image Therapeutic: (What we use) To put it simply, the ultrasound machine produces an electrical current that is converted into acoustic energy through the transducer. In order for this acoustic energy to be absorbed into the body, we use a coupling agent. This is where the blue gel comes into play. This gel decreases acoustical impedance by eliminating as much air as possible. This allows us to more effectively direct this energy to our target area Why do we use it? Therapeutic ultrasound is considered a deep heating agent, so unlike moist heat and hot pads, ultrasound can increase tissue temperature at a depth of 5 cm. This allows us to more effectively treat deep structures like muscle. Ultrasound has the potential to decrease pain, muscle spasms and joint stiffness as well as help facilitate tissue repair. We personally like to use ultrasound early on in a patient's rehabilitation when movement and exercise is contraindicated or not well tolerated. With that said, ultrasound is not indicated for everyone and their are contraindications that your therapist must screen for prior to providing treatment It’s starting to get warmer outside which means spring sports are on the horizon. With the coming of spring sports we see a lot of patients come into the clinic with pain / injuries associated with the change from winter sports to spring sports.
This week we received a great question that is featured in this weeks blog from Mary B. “Hey Tony I have two kids that play basketball in the winter and are transitioning to softball and lacrosse this spring, what are some things that I should consider.” We broke this down into 5 things to consider....
Why working out with a partner is beneficial:
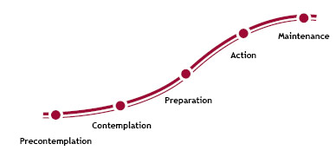
By: Dr. Elizabeth Bynum, PT, DBT  Frequently we attempt to make behavioral changes such as exercising more or eating healthier in an effort to improve our quality of life. Most individuals that attempt to do this are able to maintain the desired change for a few months. But, unfortunately, studies have shown that most people attempting to change their lifestyle fall short of maintaining the behavior change. This is primarily due to the fact that they have not set up the appropriate steps it takes to maintain a behavior change. In fact, research suggests that if you can maintain a behavior for 6 months or longer, the risk of relapsing into your old habits decreases substantially! So what does this mean for you? In order to adopt a healthier lifestyle and improve your chances of maintaining the lifestyle, you have to: 1) Surround yourself with people who support you and participate in the same activities that endorse your newly desired lifestyle. 2) Once you have hit your long term goal of a desired change, create a new long term goal to focus on. Then make more short term goals to measure your small successes along the way! 3) Self-efficacy, self-efficacy, Self-efficacy! Improving your self confidence and believing that you are capable of continuing a healthier lifestyle is extremely important and associated with a high predictability that you will continue to succeed in meeting your goals. Remember, you are stronger than you think! 4) Ensure you feel good and continue to feel good from the newly adopted change. Continuing to see impacts and positive changes will only improve your desire to continue the behavior. Make sure the benefits of your change truly outweigh the “good” feeling you got from your previous behavior. When faced with temptation, remind yourself of these heavily weighted benefits from your new habit and stick to it! 5) Continue to work on the behavior change until you no longer feel any temptation to fall back to your old habits. If you find that you no longer desire something that you couldn’t go without before, then you can be confident that your chances of relapse are extremely small. Below is a picture of a model that experts use to help guide you through a desired behavior change and the maintenance of that behavior. Remember that if you are reading this you have achieved, or, are working to achieve a goal. Determine what stage you are in, make a plan, incorporate the five steps mentioned above, and you’ll be on your way to maintaining a behavior and terminating any threats to fall back into your old ways! Pre-contemplation Phase: People in this phase are unaware of the need to change and currently have no intentions on doing so.
Contemplation Phase: People in this phase are aware of a need to change and are considering the pros and cons of moving forward with a given behavior change. Preparation Phase: In this stage, people are getting ready to make a change within ~30 days. They realize that a behavior change will positively impact their quality of life. Action Phase: People in this stage are currently participating in a desired behavior change and have been working on this change within the past 6 months. Maintenance phase: People in this stage have been adhering to a behavior change for 6 months or greater. They are working on maintaining the behavior and preventing relapse to previous stages. Best of luck and always remember that at Empire Performance PT, we are here to help you! Stop in and ask about our cash based program where we help you maintain an active lifestyle through 1 on 1 time with a doctor of physical therapy! By: Dr. Kyle Ioos, PT, DPT  Isn’t soup the best? Especially this time of the year - who doesn’t love a cup of hot, healthy goodness? They’re also so easy to make and require very little clean-up (most of the time). I find myself gravitating to creamy vegetable soups most of the time and I hardly ever follow a recipe. I throw 3-4 different veggies into a large pot, add desired spices, boil them in broth/water until tender, then add in a can or two of light coconut milk (depending on how much I’ve made) and blend it all together with an immersion blender. I also love serving it over some rice - which makes it much more filling. If I am following a recipe (or using one for a frame of reference), the first two recipes below are my go to. The third soup is one I haven’t made yet but it definitely on my Soups-To-Make list: 1. Vegan Broccoli Cheddar Soup
2. Split Pea Soup
3. Knoephla Soup Soup:
Knoephla:
Instructions: For the soup: Melt the butter in a large pot over medium-high heat. Add the carrots, celery, onions, a good pinch of salt and a few turns of pepper and cook, stirring often, until the vegetables soften, about 10 minutes. Add the garlic and nutmeg and cook, stirring, until fragrant, 2 more minutes. Stir in the stock, herbs, bay leaves and potatoes. Increase the heat to high and bring to a boil. Reduce the heat to a simmer, then cover and cook for 40 minutes. For the knoephla: Meanwhile, whisk together the flour, baking powder, salt, a few turns of pepper and the nutmeg in a medium bowl. Stir in 1 cup (236 grams) water and the egg and mix to form a shaggy dough. Turn it out onto a clean work surface and knead it for a few minutes, adding flour as needed, until you have a smooth and stiff dough. Roll it into a 1/2-inch-thick blob, then cut into 1/2- to 3/4-inch squares, dusting with flour so they don't stick together.When the soup has 20 minutes left of simmer time, add the knoephla directly to the soup and continue to simmer. Stir in the cream. Taste and adjust the seasonings as desired. Remove the bay leaves before serving. Credit If you try one of these recipes, be sure to let me know the next time you stop into the clinic! By: Chloe, Patient Success Coordinator Snowed in and can’t make it to the gym? Here are 8 exercises for a total body workout that you can do from the comfort of your own home with virtually no equipment.  Side lying hip abduction: While lying on your side, slowly raise up your top leg towards the sky. Keep your knee straight and maintain your toes pointed forward the entire time. Keep your leg in-line with your body. Perform 3 sets of 10 to 15 repetitions.  Squats: Stand with feet shoulder width apart and toes pointed forward to slightly turned out. Bend knees and lower buttock towards floor keeping your back straight and bending at your hips. Perform 3 sets of 10 to 15 repetitions.  Good mornings: Stand with your feet hip-width apart, and place your hands at the back of your head with your elbows opened wide. Pull your abs to your spine, and keep your back neutral while pressing your butt backward, hinging at the hips, until your back is almost parallel to the floor. Keep a slight bend in your knees as you bend forward. Return to standing, squeezing your glutes when you are upright. Perform 3 sets of 10 to 15 repetitions  Calf raises off of a step: While standing on the edge of a step with your heels off the back end of the step, raise up on your toes as you raise your heels and body upward as shown. Perform 3 sets of 10 to 15 repetitions.  Push ups: Select one of the above push ups based on your ability. Perform 3 sets of 10 to 15 repetitions.
 Plank: While lying face down, lift your body up on your elbows and toes. Try and maintain a straight spine. Hold this position for 60 seconds and repeat 3 times. If you are unable to maintain a straight spine for the full 60 seconds, you can either start with less time per set or try a plank from the kneeling position seen below. |
AuthorDr. Tony Tanzi: Physical Therapist, Triathlete, Runner, Performance Coach Archives
October 2022
Categories |








 RSS Feed
RSS Feed